Controlling diabetes is crucial for preventing complications and maintaining a healthy life. Effective diabetes management involves a combination of lifestyle changes, medication, and regular monitoring. Here’s a comprehensive guide to managing and controlling diabetes:
- Healthy Eating:
Balanced Diet: Focus on a diet rich in vegetables, whole grains, lean proteins, and healthy fats. Limit refined carbohydrates, sugary foods, and processed snacks.
Carbohydrate Counting: For those with Type 1 diabetes or insulin-dependent Type 2 diabetes, counting carbohydrates helps manage blood sugar levels by matching insulin doses to carb intake.
Portion Control: Eating smaller, consistent portions can help prevent blood sugar spikes and maintain steady glucose levels.
Glycemic Index: Choose foods with a low glycemic index (GI), as they have a slower effect on blood sugar levels. - Regular Physical Activity:
Exercise Routine: Aim for at least 150 minutes of moderate-intensity aerobic exercise (such as brisk walking, cycling, or swimming) per week, combined with strength training twice a week.
Blood Sugar Monitoring: Check blood sugar before and after exercise, especially if you take insulin or medications that can cause hypoglycemia.
Stay Active: Incorporate physical activity into your daily routine, such as taking stairs instead of elevators or walking short distances instead of driving. - Medication Management:
Insulin: For those who need insulin, take it as prescribed, and adjust doses based on blood sugar readings, meals, and activity levels.
Oral Medications: Take diabetes pills as prescribed by your healthcare provider. Common medications include metformin, sulfonylureas, and DPP-4 inhibitors.
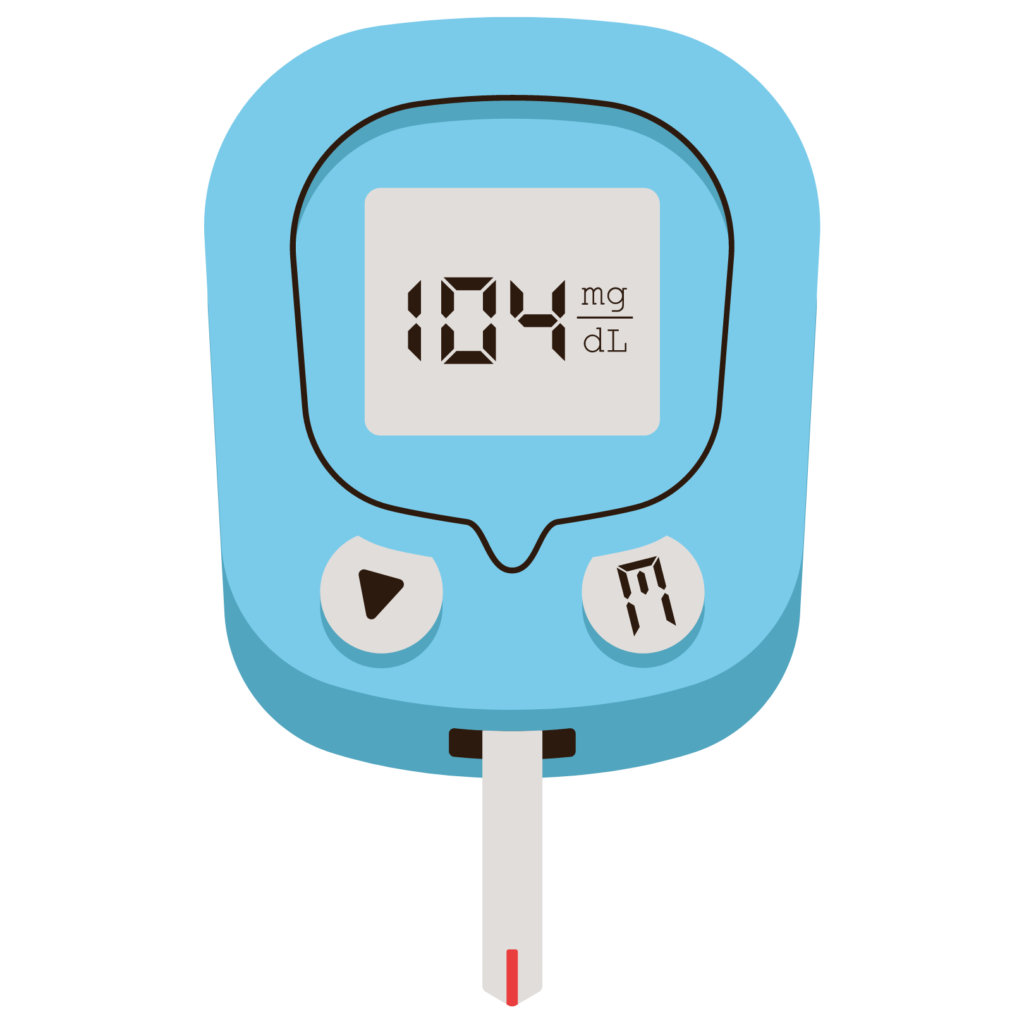
Newer Medications: Some people may be prescribed newer classes of medications like GLP-1 receptor agonists or SGLT2 inhibitors, which can help with blood sugar control and weight management. - Blood Sugar Monitoring:
Regular Testing: Check your blood sugar levels as recommended by your healthcare provider. This helps you understand how food, activity, and medication affect your glucose levels.
Continuous Glucose Monitoring (CGM): CGM systems provide real-time glucose readings and can alert you to high or low blood sugar levels.
HbA1c Testing: This blood test shows your average blood sugar levels over the past 2-3 months. Aim for a target HbA1c level as advised by your doctor, usually below 7%. - Weight Management:
Healthy Weight: Maintaining a healthy weight is crucial for controlling Type 2 diabetes. Even a modest weight loss of 5-10% can significantly improve blood sugar control.
Diet and Exercise: Combine a healthy diet with regular exercise to achieve and maintain your weight goals.
Medical Support: In some cases, medication or bariatric surgery may be recommended to help with weight loss. - Stress Management:
Relaxation Techniques: Practice stress-reducing activities such as meditation, deep breathing exercises, yoga, or tai chi.
Sleep: Ensure you get enough restful sleep, as poor sleep can negatively affect blood sugar levels.
Counseling: Consider talking to a counselor or joining a support group if stress or emotional issues impact your diabetes management. - Preventive Care:
Regular Check-ups: Visit your healthcare provider regularly to monitor your diabetes and screen for complications like heart disease, kidney problems, and nerve damage.
Foot Care: Check your feet daily for any cuts, blisters, or signs of infection, as diabetes can cause poor circulation and nerve damage.
Eye Care: Have an annual dilated eye exam to check for diabetic retinopathy, a condition that can lead to vision loss.
Vaccinations: Stay up-to-date with vaccines, including flu and pneumonia shots, as diabetes can make infections more severe. - Avoiding Complications:
Manage Blood Pressure: Keep your blood pressure under control (below 140/90 mm Hg or as recommended by your doctor).
Cholesterol Control: Manage cholesterol levels with a heart-healthy diet, exercise, and medications if needed.
Quit Smoking: Smoking increases the risk of diabetes complications. Seek support to quit smoking if you are a smoker. - Education and Support:
Diabetes Education: Participate in diabetes self-management education programs to learn more about managing your condition.
Support Networks: Engage with support groups, either in-person or online, to share experiences and gain support from others with diabetes. - Regular Monitoring and Adjustments:
Adjustments: Regularly review and adjust your diabetes management plan with your healthcare provider, especially if your lifestyle changes or if you experience new symptoms.
Stay Informed: Keep yourself informed about the latest diabetes management strategies and advancements.
Controlling diabetes requires a proactive and comprehensive approach. By staying informed, making healthy choices, and working closely with your healthcare team, you can manage your diabetes effectively and live a healthy, fulfilling life.
